Rural Mental Health
For immediate mental health needs, please contact one of these hotlines:
- 988 Suicide and Crisis Lifeline
24/7 - 2-1-1, a comprehensive hotline that connects callers with local resources
According to the Results from the 2022 National Survey on Drug Use and Health: Detailed Tables, approximately 7.7 million nonmetropolitan adults reported having any mental illness (AMI) in 2022, accounting for 23.0% of nonmetropolitan adults. In addition, 1.9 million, or 5.7%, of adults in nonmetropolitan areas reported having serious thoughts of suicide during the year.
While the prevalence of mental illness is similar between rural and urban residents, the services available can be very different. Mental healthcare needs are often not met in many rural communities across the country because adequate services are not present. Providing mental health services can be challenging in rural areas. According to the National Rural Health Association, the following factors are particular challenges to the provision of mental health services in rural communities:
- Accessibility – Rural residents often travel long distances to receive services, are less likely to be insured for mental health services, and providers are less likely to recognize a mental illness.
- Availability – Chronic shortages of mental health professionals exist and mental health providers are more likely to practice in urban centers.
- Affordability – Some rural residents may not be able to afford the cost of health insurance or the cost of out-of-pocket care if they lack health insurance.
- Acceptability – Rural residents may be more susceptible to the stigma of needing or receiving mental healthcare in small communities where everyone knows each other and fewer choices of trained professionals can lead to a lack of faith in confidentiality, as well as a reliance on the informal care of family members, close friends, and religious leaders.
This topic guide focuses on mental health in rural areas and helps health and human services providers in their efforts to develop, maintain, and expand mental health services in rural communities. It also highlights challenges and important issues in mental healthcare delivery, such as workforce shortages, access issues, anonymity, stigma, integration of mental health services into primary care, and suicide prevention. Information regarding substance use disorder (SUD) can be found in RHIhub's Substance Use and Misuse in Rural Areas topic guide.
Frequently Asked Questions
- Where can I find mental health statistics for rural populations?
- What are the workforce challenges in providing rural mental health services?
- What other challenges affect access and the provision of mental health services in rural areas?
- What can a rural community or healthcare facility do to minimize the challenges of accessing and providing mental health services in a rural area?
- What are some of the benefits of integration of mental health services into primary care in a rural community?
- How has COVID-19 affected rural mental healthcare access and outcomes?
- Is there a resource for rural primary care providers and other healthcare professionals that can connect patients to mental health services and treatment?
- Where can rural veterans and rural healthcare providers assisting veterans find information about mental health services in their rural areas?
- What is the impact of suicide in rural America?
- How can our community take action to prevent suicides?
- What resources are available for suicide prevention efforts?
- How can our school take action to prevent suicides?
Where can I find mental health statistics for rural populations?
On the national level, the Substance Abuse and Mental Health Services Administration (SAMHSA) is the primary source of information on behavioral health and provides an annual survey of detailed data by geographic location on the prevalence of several behavioral health measures in their annual National Survey on Drug Use and Health.
Topics with data applicable to rural mental health include:
- Mental illness in the past year
- Co-occurring mental illness with substance use disorder
- Serious mental illness
- Mental health treatment/counseling
- Unmet mental health needs
- The incidence/prevalence of serious thoughts of suicide
The data for these topics are available by age, geographic characteristics and socioeconomic characteristics. The geographic characteristics are detailed by geographic region of the U.S. and county type. County type is divided into population data classes:
- Large metro – population of 1 million or more
- Small metro – population of 50,000 – 999,999
- Nonmetro – includes subcategories:
- Urbanized – population of 20,000 – 49,999 in urbanized areas
- Less urbanized – population of 2,500 – 19,999 in urbanized areas
- Completely rural – population of < 2,500 in urbanized areas
RHIhub's Finding Statistics and Data Related to Rural Health provides additional resources related to behavioral health data.
What are the workforce challenges in providing rural mental health services?
According to a 2018 study, the most significant challenge preventing rural Americans from receiving care is the lack of mental health professionals providing mental health services in rural and frontier areas.
To further complicate the challenges of providing mental health services, the most disadvantaged and under-resourced communities are often those with the greatest need for mental healthcare providers.
As of September 30, 2021, HRSA had designated 3,426 Mental Health Professional Shortage Areas in rural areas. It is estimated that it would take 1,597 practitioners to remove the designations. For the most current figures, see HRSA's Designated HPSA Statistics.
This map identifies nonmetro Mental Health HPSAs based on April 2024 data.HRSA.gov data:
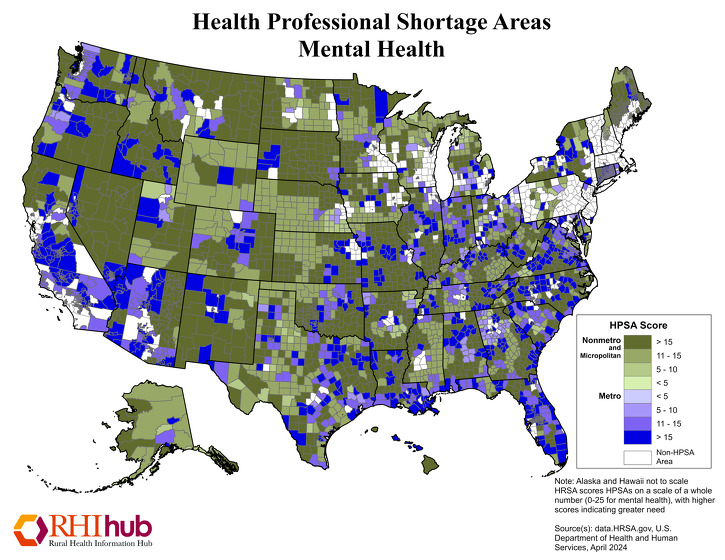
The data.HRSA.gov interactive map of Mental Health Professional Shortage Areas (HPSA) identifies the total number and geographic location of Mental Health HPSAs by state and county.
What other challenges affect access and the provision of mental health services in rural areas?
Travel distance, lack of public transportation, and the lack of health insurance covering mental health services are commonly identified as challenges to accessing healthcare in rural areas. Reimbursement issues and the social stigma associated with mental health services are also identified as significant challenges that affect access and the provision of mental health services in rural areas.
Reimbursement
The reimbursement offered by payers such as Medicaid, Medicare, and private insurers has a significant impact on the ability of rural providers to offer mental health services. The publication Encouraging Rural Health Clinics to Provide Mental Health Services: What are the Options? notes that Rural Health Clinics may be reluctant to start providing mental health services when reimbursement rates are low. In addition, high no-show rates among mental health clients and high numbers of uninsured patients further exacerbate the issue of low reimbursement rates paid by Medicaid and others.
Providing mental health services via telehealth, sometimes referred to as telemental health or telebehavioral health, has shown promise in helping to alleviate the lack of mental health services in rural areas. However, reimbursement is also a challenge for telehealth services. For additional information about telehealth services and associated reimbursement issues, see RHIhub's Telehealth and Health Information Technology in Rural Healthcare topic guide.
Stigma
Nearly 1 in 5 adults in the U.S. experiences a mental disorder within any given year according to the National Alliance on Mental Illness. Yet, the misconceptions, myths, and cultural stigma associated with mental illness are significant barriers that keep people with mental health disorders from seeking and receiving treatment in rural areas. Factors that may influence rural residents to avoid seeking care include such issues as:
- Lack of understanding and knowledge of mental illness, sometimes even among healthcare staff
- Prejudice or stigma towards people with mental health disorders, often based on fear and unease
- Secrecy about mental illness in the community and general hesitancy to seek care
- Perception of a lack of confidentiality and privacy in small towns with closely-tied social networks
While there are drawbacks to small communities when it comes to mental health, there are positives as well. The close-knit nature of rural communities can also mean that residents are more likely to rally around each other and provide community support in times of need. A strong external support group can help facilitate a person's success in treatment and also help support the family's efforts in attending to the care seeker.
What can a rural community or healthcare facility do to minimize the challenges of accessing and providing mental health services in a rural area?
There are several approaches that can be tried in rural communities to minimize the challenges of providing mental health services and expanding the mental health workforce. Some of the most commonly cited practices to deal with workforce issues include:
- Expanding the use of telemental health services
- Offering loan repayment programs and state tax waivers to recent behavioral health professions graduates
- Providing clinical rotations in a rural setting to expose future health care professionals to the qualities of working in rural areas
Another approach to improving access and providing mental health services is the School-Based Health Center (SBHC) model for children in rural areas. SBHCs work with the school and community to improve children's mental health by providing onsite healthcare services delivered by an interdisciplinary team of primary care and behavioral health clinicians. Services may range from wellness exams to mental health services. SBHCs can screen children for mental, behavioral, or developmental disorders (MBDDs) including anxiety, depression, and attention-deficit/hyperactivity disorder (ADHD). In addition, SBHCs can provide customized care for children with special needs who may be at a higher risk for MBDDs by monitoring medication and assisting in developing Individualized Education Plans (IEPs).
In addition, education and awareness efforts targeted toward rural residents have been used to increase familiarity and comfort with mental health issues. An example of this is the Mental Health First Aid public education program. This program helps rural residents identify, understand (and thereby reduce the stigma), and respond to signs of mental illnesses and substance use disorders.
What are some of the benefits of integration of mental health services into primary care in a rural community?
In recent years, health policy experts and healthcare providers have begun to encourage closer integration of mental or behavioral health and primary care services. It is assumed that integration will increase access to mental healthcare services, particularly in rural communities, as well as increase quality of care through enhanced coordination of services. In rural areas, where behavioral health workers and primary care providers are in short supply, integration is vitally important. Integration of these services is an effective strategy for maximizing the use of scarce rural healthcare resources and improving the quality of care for both behavioral health and primary care patients.
According to a 2010 Maine Rural Health Research Center report, patients in rural areas who need mental health services typically see their primary care provider first. Often it is the primary care provider who initially diagnoses the need for mental health services. In addition, a high percentage of mental healthcare for rural patients is already provided by primary care providers, so integrating the services of a mental healthcare provider into the primary care setting can expand on what is already being done. Efficiency of service and ease of use also create a level of coordinated care and access that benefits both the patient and the provider.
The integration, or even the co-location, of mental health services with primary care services can also help to reduce or eliminate the effects of the powerful social stigma associated with mental illness in many rural areas. Social stigma prevents many rural citizens from obtaining needed services, but it is less of a deterrent when behavioral health professionals see patients in primary care settings. The integration of behavioral health and primary care services also reduces the challenge of maintaining anonymity. Rural patients may be reluctant to be seen in settings where their privacy might be compromised but more willing to seek mental healthcare from the more common and accepted primary care clinic. Primary Care, Behavioral Health, Provider Colocation, and Rurality discusses how co-location, although different from integration, offers the potential of future collaboration with primary care providers, as well as opportunities for care coordination.
For additional information about integration of mental health services into primary care, see The Future of Rural Behavioral Health and A Guidebook of Professional Practices for Behavioral Health and Primary Care Integration: Observations from Exemplary Sites, and for information about co-location of mental health services with primary care see Primary Care, Behavioral Health, Provider Colocation, and Rurality.
See Tri-Area Community Health Provides Community-Focused Integrated Care in RHIhub's Rural Monitor for a successful example of integration in southwestern Virginia. In addition, several promising examples of integrated service delivery are available in RHIhub's Rural Health Models and Innovations.
How has COVID-19 affected rural mental healthcare access and outcomes?
The COVID-19 pandemic and the resulting social and economic upheaval have affected health outcomes and healthcare access in rural communities across the nation. Mental health is no exception. According to a 2020 CDC MMWR report, approximately 30% of rural adults who responded to a survey suffered from anxiety or depression and approximately 10% seriously considered suicide in the past 30 days in June of 2020.
This has led to an increase in demand for mental health services in rural areas that were already experiencing significant provider shortages. Across the country, many mental health services transitioned to telehealth, which has created both opportunities and challenges for rural communities. According to a 2021 report, 43% of rural adults who received behavioral health treatment over the last year said they used telehealth at least once a month. Telehealth options allowed many rural residents to maintain their treatment, and in some cases improved the convenience of access to those services. However, in some rural and remote areas lacking broadband access, video-based telehealth was not feasible. On March 1, 2020, as a provision of the CARES Act, CMS waived the video requirement during the Public Health Emergency, allowing telehealth to be conducted via audio-only sessions. A July 2020 article from the Commonwealth Fund highlights that the overall lack of mental health providers, combined with the increased demand for services due to the pandemic, has made access to mental health services difficult regardless of telehealth capabilities, as many mental health providers were already operating at full or nearly full capacity before the pandemic began.
The pandemic also had a significant effect on the economy. Many of the workers who lost their jobs due to the pandemic also lost health insurance coverage. According to a report from the UDSA-ERS, the unemployment rate in rural areas rose from 4.9% in March 2020 to 13.6% in April. A 2021 study of COVID-19's impact on the well-being of rural communities in the West found that 21% of people who had previously been employed full-time had lost that status due to the pandemic. Roughly half of those who lost full-time jobs became temporarily unemployed and around 28% had shifted to part-time work. For part-time workers, 41% changed status, and 73% of these former part-time workers were temporarily unemployed. Of those surveyed for this study, 44% reported that the pandemic caused some level of negative impact to their mental health.
A similar study on mental health and work status in rural Appalachia found that 66% of people surveyed suffered from at least one mental health issue during the pandemic, such as isolation/loneliness, depression, hopelessness, or anxiety. Of the various types of workers who reported suffering from mental health issues, the highest percentage (69%) were workers who switched from in-person to remote work during the shutdown. The workers who continued to work outside the home, however, were more likely to face reduced income.
Is there a resource for rural primary care providers and other healthcare professionals that can connect patients to mental health services and treatment?
When there are few resources to provide direct mental health services in a community, local healthcare professionals may need to refer patients to facilities outside of the community. The Substance Abuse and Mental Health Services Administration (SAMHSA) maintains a Behavioral Health Treatment Services Locator, which helps locate mental health services in your area, and the National Directory of Mental Health Treatment Facilities 2020, an online listing of federal, state and local government, and private facilities that provide mental health treatment services.
Where can rural veterans and rural healthcare providers assisting veterans find information about mental health services in their rural areas?
Rural healthcare providers and veterans can find information about mental health services for veterans in their area by contacting either their closest VA medical center or community-based outpatient clinic (CBOC). To access contact information, go to the VA Locations tool and choose a state to access a list of CBOCs, VA Medical Centers, and Vet Centers. See the VA Mental Health website for a broad overview of mental health programs available to veterans. Additional information can be found in the Guide to VA Mental Health Services for Veterans & Families.
What is the impact of suicide in rural America?
Suicide is a major public health concern across the U.S. According to Understanding the Impact of Suicide in Rural America, suicide continues to be higher in rural counties and the gap between rural and urban suicides has widened over time. A 2017 CDC report, Trends in Suicide by Level of Urbanization — United States, 1999–2015, discusses possible causes for the geographic disparity: limited access to mental healthcare, social isolation, the opioid overdose epidemic, and the economic recession. Included in the report is this chart showing how the disparity has widened in recent years:
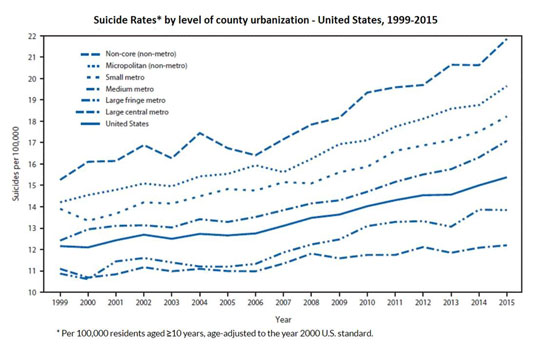
According to a 2020 report from the CDC, from 2000 to 2018, the rural suicide rate increased by 48% while urban rates increased by 34%. In 2018, the suicide rate in rural counties was 19.4 deaths per 100,000 compared with urban counties at 13.4 deaths per 100,000.
The following table presents National Vital Statistics System (NVSS) data for suicide deaths and death rates per 100,000 for 2013-2015.
| Characteristic | Large metropolitan |
Medium/
metropolitan |
Nonmetropolitan/ rural |
|---|---|---|---|
| County Urbanization | 12.72 | 16.77 | 19.74 |
| Sex | |||
| Male | 20.20 | 26.68 | 31.62 |
| Female | 5.91 | 7.51 | 8.06 |
| Race/Ethnicity | |||
| White, non-Hispanic | 17.24 | 20.24 | 21.96 |
| Black, non-Hispanic | 6.56 | 6.89 | 6.07 |
| American Indian/
|
14.00 | 19.60 | 29.07 |
| Asian/Pacific Islander, non-Hispanic | 6.70 | 8.35 | 9.35 |
| Hispanic | 6.37 | 7.97 | 10.21 |
| Source: Suicide Trends Among and Within Urbanization Levels by Sex, Race/Ethnicity, Age Group, and Mechanism of Death — United States, 2001–2015. MMWR Surveillance Summaries, 66(18);1–16, 2017 | |||
Additional information regarding the impact of suicide in rural communities can be found in Understanding the Impact of Suicide in Rural America. This policy brief developed by the National Advisory Committee on Rural Health and Human Services (NACRHHS) also discusses prevention strategies available at the state and national level and provides recommendations to the Department of Health and Human Services urging it “to focus more explicitly on emphasizing and including the rural dimensions of suicide into their programs, research, and outreach to address existing knowledge gaps and strengthen the evidence base.”
How can our community take action to prevent suicides?
The Suicide Prevention Resource Center (SPRC) is a premiere source of information on the topic of suicide prevention. The following resources and tools can be helpful to rural communities working on suicide prevention efforts:
- Suicide Prevention Toolkit for Primary Care Practices – A toolkit that contains information, resources, and tools to implement suicide prevention practices in primary care, including rural settings.
- States and Communities – Find out what your state is doing to prevent suicide. Includes state suicide prevention plans, state data, and how to contact people involved in suicide prevention in your state.
- Engaging People with Lived Experience: A Toolkit for Organizations – A toolkit for building community suicide prevention programs informed by the lived experience of community members who's lives have been directly impacted by suicide.
You can also contact the Suicide Prevention Resource Center for assistance. SPRC can connect you with people, organizations, and resources in your rural community, state and nationally and provide technical assistance and training on suicide prevention.
For more information on how to develop a suicide prevention program, see the Rural Suicide Prevention Toolkit.
What resources are available for suicide prevention efforts?
The U.S. Department of Health and Human Services (HHS) considers suicide a significant public health problem and is involved in prevention activities. Several federal agencies collaborate and direct necessary prevention resources, services, and programs that are both public and private. Federal resources on suicide prevention include:
- Suicide Prevention, Centers for Disease Control and Prevention
- Suicide Prevention, National Institutes of Health
- Preventing Suicide, Substance Abuse and Mental Health Services Administration
- National Strategy for Suicide Prevention: Goals and Objectives for Action, U.S. Surgeon General
- Tribal Training and Technical Assistance Center, Substance Abuse and Mental Health Services Administration
In addition to the resources provided by the federal government and the Suicide Prevention Resource Center, these organizations also provide additional suicide prevention information:
-
American Association of Suicidology
202.237.2280 -
American Foundation for Suicide Prevention
888.333.2377 -
National Action Alliance for Suicide Prevention
202.572.3784 -
National Institute of Mental Health –
Suicide Prevention
866.615.6464 -
988 Suicide and Crisis Lifeline
Contact by email for information and resources
How can our school take action to prevent suicides?
According to the Centers for Disease Control and Prevention, suicide is the second leading cause of death among youth (ages 10-24) in America. Rural schools can play an important role in preventing suicide among rural youth by:
- Becoming involved with your state or community's suicide prevention coalition to learn how to coordinate your school's efforts with state or community efforts.
- Visiting SPRC's Customized Information pages for Teachers and School Mental Health Providers to learn more about how to respond to students and staff at risk for suicide.
-
Implementing a school-based suicide prevention program, which includes a comprehensive set of interventions,
such as:
- Gatekeeper training
- Screening for mental health
- Health education curriculum that includes suicide prevention and/or mental health
- Peer mentoring
- School-based mental health services
- Crisis response
- Postvention
Also, the National Association of School Psychologists webpage Preventing Youth Suicide provides a variety of prevention resources for school administrators, crisis teams, educators, and parents. - Creating a postvention plan for your school with assistance from AFSP/SPRC's After a Suicide: A Toolkit for Schools, Second Edition.
- Offering a Mental Health First Aid training program in your rural community for individuals to learn how to help people who are in a crisis.
To review guidelines for school-based suicide prevention programs, please refer to the University of South Florida's Youth Suicide Prevention School-Based Guide. The guide also includes tips on responding following a suicide or suicide attempt in the school community. For more information on any of the items listed above, please visit the SPRC Online Library or contact one of the SPRC Prevention Specialists.



